MAKE THE CONNECTION between SARDs and ILD
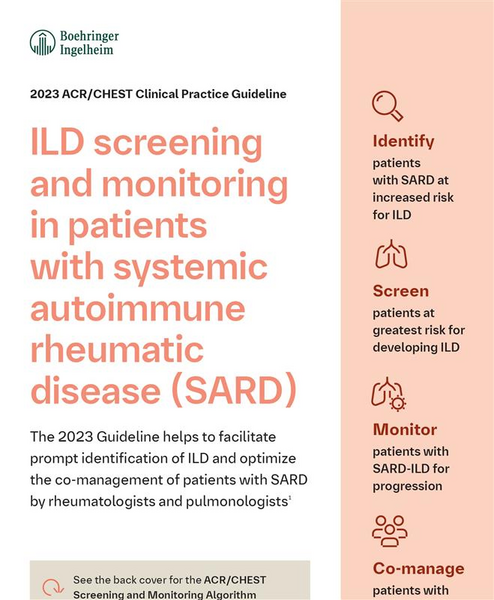
As a rheumatologist, you play an important role in the co-management of SARD-ILD, helping in early identification, monitoring and screening, and remaining part of the on-going multidisciplinary team.1
Overview of the ACR/CHEST Guideline for Screening and Monitoring of ILD in SARDs
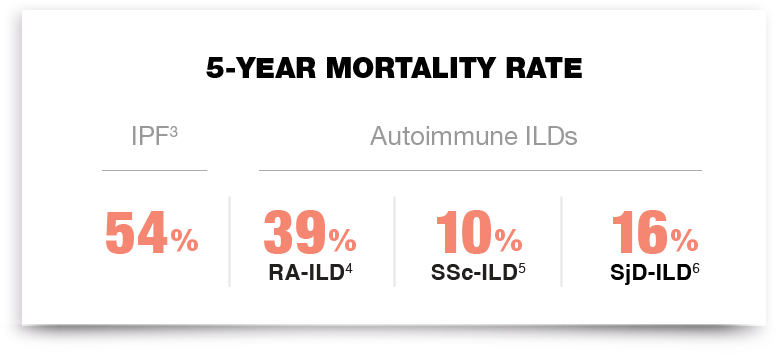
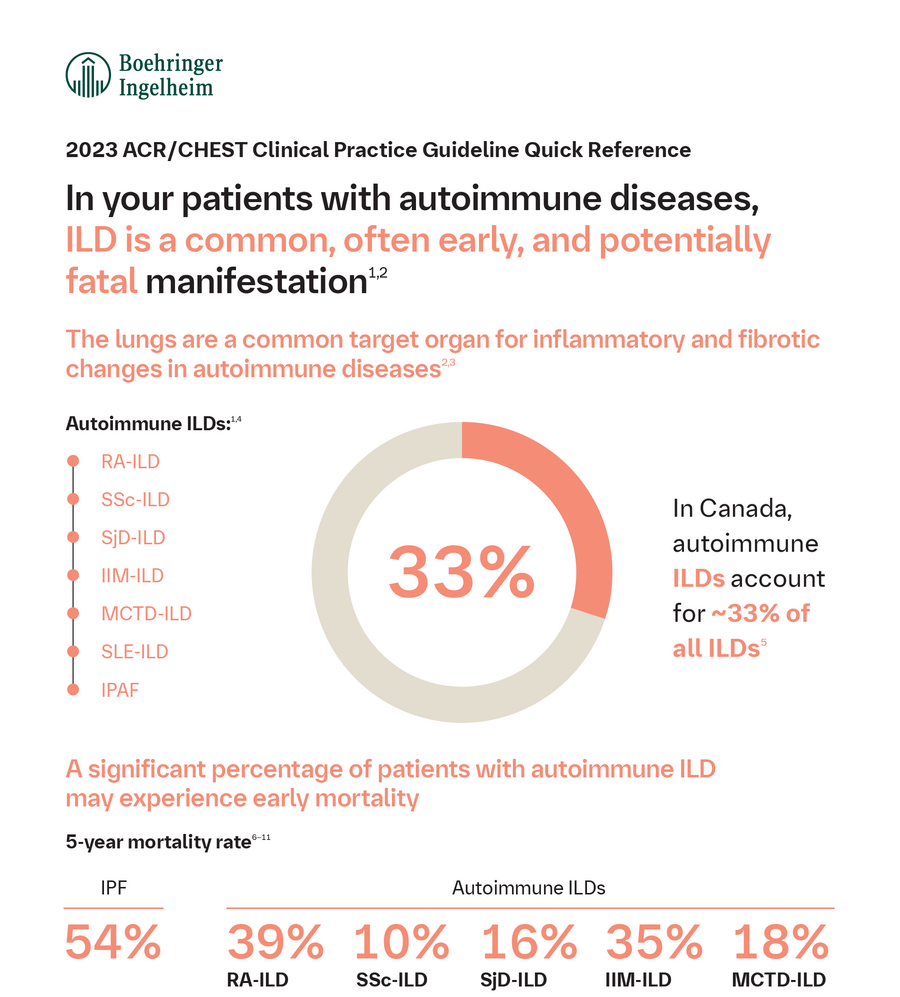
KNOW the threat of SARD-ILD2
Interstitial lung disease (ILD) is a common, often early, and potentially fatal manifestation in patients with systemic autoimmune rheumatic diseases (SARDs).1,2
IDENTIFY patients with SARDs at risk for ILD2
Some disease features increase the risk of developing ILD, for example:
Disease | Risk factors for developing ILD* |
RA |
|
SSc |
|
SjD |
|
Adapted from Johnson SR, et al. Arthritis Rheumatol 2024.
The ACR/CHEST Guideline recommends screening patients with SARDs at increased risk for ILD2
To review the complete ACR/CHEST Guideline for the Screening and Monitoring of ILD in People with SARDs, click here.
SCREEN patients identified as being at risk of ILD2
Diagnostic and screening interventions:
In all patients with SARDs, listen for “Velcro®-like” crackles during routine physical examination2,7†‡
Screen with PFTs if ILD risk is identified, followed by a chest HRCT if ILD is suspected2
Screening should not be limited to those with risk factors and should be performed if there is any uncertainty regarding whom to screen2
If you suspect ILD or ILD is detected, refer your patient to a respirologist indicating ILD is suspected and provide diagnostic evidence (e.g., PFTs, HRCT, etc.), if available.7,8
LISTEN for the one sound that may suggest ILD: inspiratory fine crackles†
Features of dry inspiratory crackles:7,9,10
- Typically heard at the lung bases on the posterior chest (back)
- Heard during middle to late inspiration
- Short duration and does not clear with cough
- Sounds like VELCRO® Brand Fastener‡ being peeled apart

Prompt diagnosis by a multi-disciplinary team of specialists can help ensure patients receive the appropriate care and support
DISCOVER HOW AND WHY IDENTIFYING SARD-ILDs MATTERS
Downloadable resources for rheumatologists:
ACR/CHEST Guideline:
SARD-ILD Overview
ACR/CHEST Guideline:
SARD-ILD Summary Tool

Guideline Criteria for Identifying PPF in ILD
To review the complete ATS Guideline on IPF and PPF in Adults, click here.
Downloadable resources for your patients:

RA-ILD Symptom Tracker
Understanding and Living with RA-ILD

Understanding and Living with SSc-ILD
RA-ILD=rheumatoid arthritis-interstitial lung disease; SSc-ILD=systemic sclerosis-interstitial lung disease; SjD-ILD=Sjögren’s disease-interstitial lung disease; IPF=idiopathic pulmonary fibrosis; ACR=American College of Rheumatology; CHEST=American College of Chest Physicians; RA=rheumatoid arthritis; RF=rheumatoid factor; CCP=cyclic citrullinated peptide; SSc=systemic sclerosis; SjD=Sjögren’s disease; PFT=pulmonary function test; HRCT=high-resolution computed tomography; PPF=progressive pulmonary fibrosis.
* These disease features have been identified as placing a person at increased risk for developing ILD; however, the absence of these risk factors does not preclude the development of ILD in patients with these SARDs. Screening for ILD should be performed in shared decision-making with the rheumatologist and patient. As such, screening for ILD should not necessarily be limited only to those with these risk factors.
† Lung auscultation should be part of the initial screening; however, it does not take the place of PFTs and chest HRCT.
‡ VELCRO® is a registered trademark. Used with permission.
-
Fischer A and Distler J. Clin Rheumatol 2019;38(10):2673–81.
-
Johnson SR, et al. Arthritis Rheumatol 2024. doi: 10.1002/art.42860. Online ahead of print.
-
Zheng Q, et al. ERJ Open Res 2022;8:00591-2021.
-
Hyldgaard C, et al. Ann Rheum Dis 2017;76(10):1700–6.
-
Bouros D, et al. Am J Respir Crit Care Med 2002;165(12):1581–6.
-
Ito I, et al. Am J Respir Crit Care Med 2005;171(6):632–8.
-
Zibrak JD and Price D. NPJ Prim Care Respir Med 2014;24:1–4.
-
Johannson KA, et al. Can J Respir Crit Care Sleep Med 2017;1(3):133–41.
-
Ryu RH, et al. Mayo Clin Proc 2007;82(8):976–86.
-
Sgalla G, et al. BMC Pulm Med 2018;18(1):103.

