While all patients with IPF have progressive pulmonary fibrosis, there exists a variety of other ILDs that may also develop a progressive fibrosing ILD1–3
Pulmonary fibrosis is common to many ILDs1

ILDs are a diverse group of more than 200 heterogeneous lung disorders4

Inflammatory and fibrotic mechanisms can coexist as drivers of ILD disease progression5
Fibrotic ILD represents a large group of pulmonary disorders that are often progressive and associated with high morbidity and early mortality5
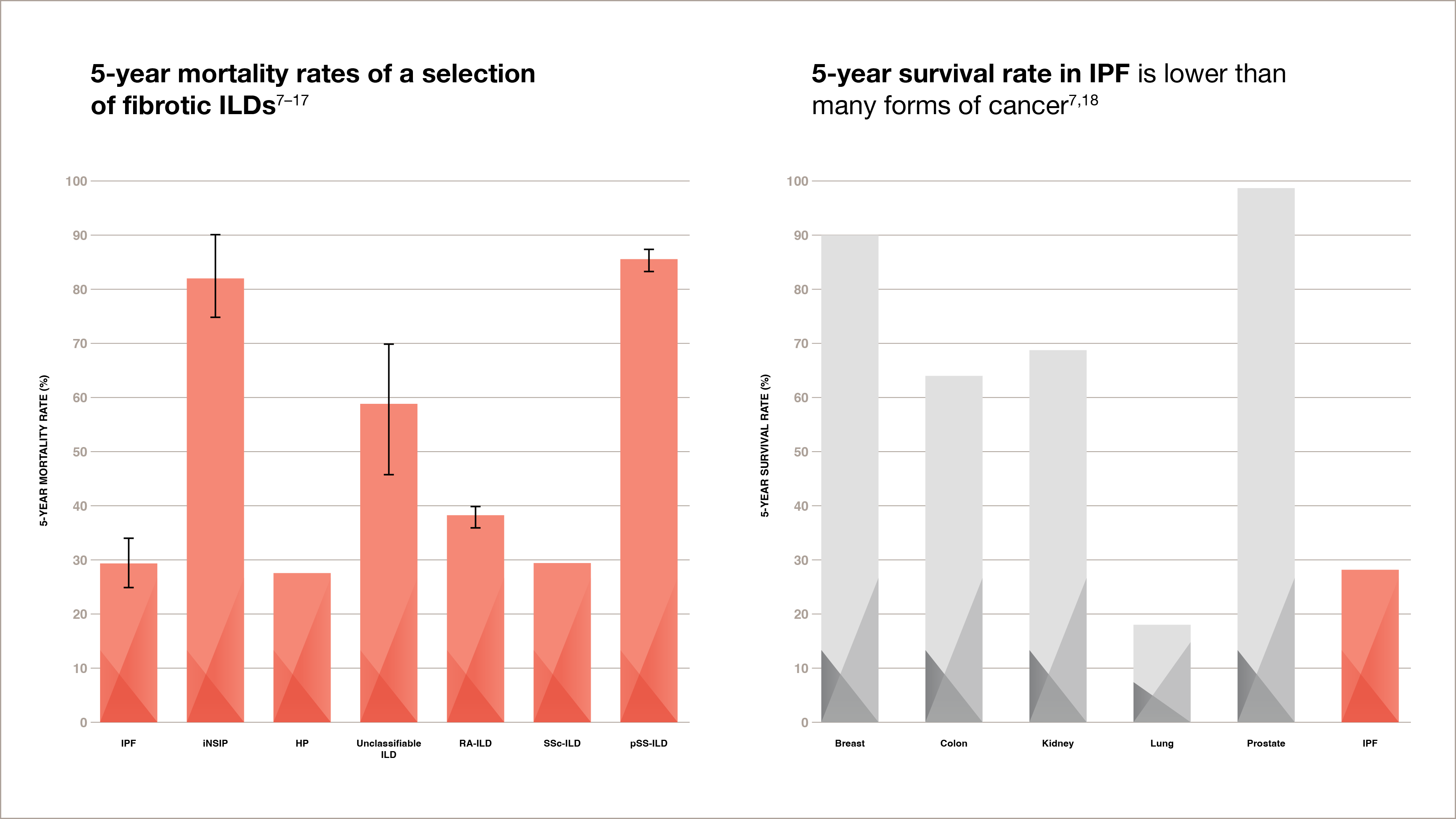
5-year mortality rates of a selection of fibrotic ILDs7–17
Bar graph showing 5-year mortality rates of a selection of ILDs, which are:
-
IPF: 25% to 34%
-
iNSIP: 74% to 90%
-
HP: 27%
-
Unclassifiable ILD: 46% to 70%
-
RA-ILD: 35.9% to 39%
-
SSc-ILD: 29.5%
-
pSS-ILD: 84% to 87.3%
5-year survival rate in IPF is lower than many forms of cancer7,18
Bar graph showing the 5-year mortality rate of IPF vs. some cancers:
-
Prostate: 97%
-
Breast: 90%
-
Kidney: 75%
-
Colon: 64%
-
IPF: 27%
-
Lung: 21%
Adapted from Vancheri et al., Park et al., Hyldgaard et al., Raimundo et al., Bouros et al., Ito et al.,
Enomoto et al., Guler et al. 2018, Vourlekis et al. 2004, and Nasser et al. 2020.
Adapted from Vancheri et al.
Patients with CTDs are at risk of developing an ILD4
Relative prevalence of ILDs and CTD-ILDs, and proportion estimates of patients who develop a progressive fibrosing disease course6
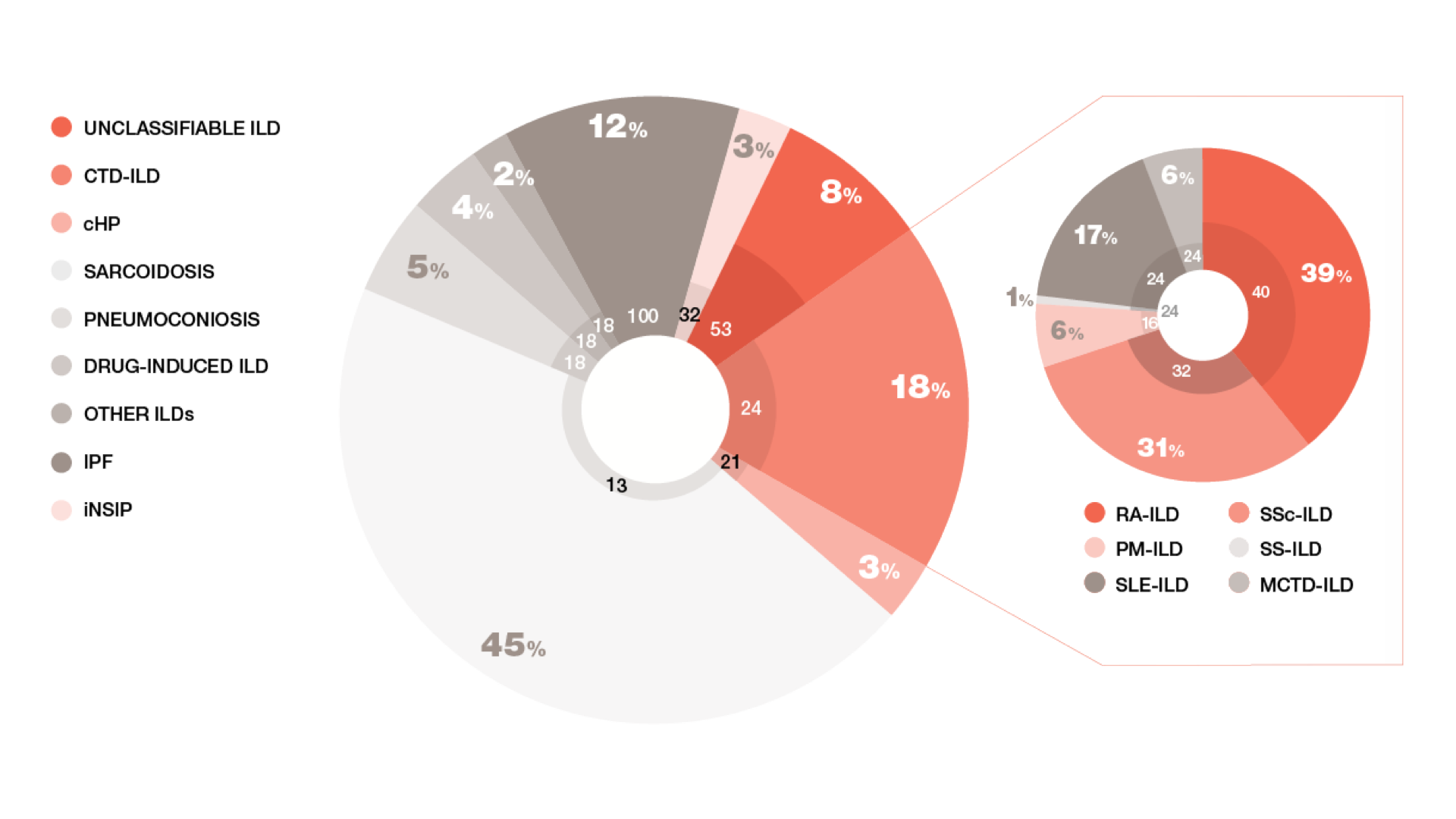
Adapted from Wijsenbeek, et al.
Relative prevalence of ILDs and CTD-ILDs, and proportion estimates of patients who develop a progressive fibrosing disease course6
A pie graph showing the proportional estimates of ILD patients who will develop a progressive fibrosing disease course, which are:
-
Unclassifiable ILD: 8% (53% with progressive fibrosis)
-
CTD-ILD: 18% (24% with progressive fibrosis)
-
cHP: 3% (21% with progressive fibrosis)
-
Sarcoidosis: 45% (13% with progressive fibrosis)
-
Pneumoconiosis: 5% (18% with progressive fibrosis)
-
Drug-induced ILD: 4% (18% with progressive fibrosis)
-
Other ILDs: 2% (18% with progressive fibrosis)
-
IPF: 12% (100% with progressive fibrosis)
-
iNSIP: 3% (32% with progressive fibrosis)
The following are a subset of the CTD-ILD 18% portion of the pie graph:
-
RA-ILD: 39% (40% with progressive fibrosis)
-
PM-ILD: 6% (16% with progressive fibrosis)
-
SLE-ILD: 17% (24% with progressive fibrosis)
-
SSc-ILD: 31% (32% with progressive fibrosis)
-
SS-ILD: 1% (24% with progressive fibrosis)
-
MCTD-ILD: 6% (24% with progressive fibrosis)
Pulmonary fibrosis can add to the burden of CTDs,
including systemic sclerosis ILD, with symptoms
that have a devastating effect on a patient’s
ability to perform activities of daily living,
significantly decreasing quality of life and
emotional wellbeing.19,20
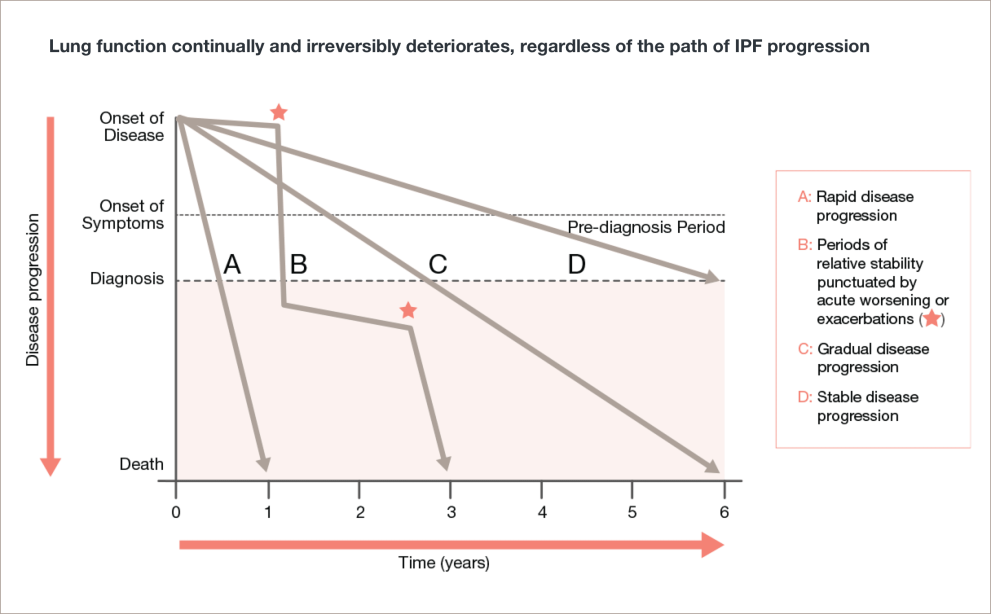
In IPF, lung function declines regardless of the clinical course of disease progression5
Adapted from Ley, et al.
Lung function continually and irreversibly deteriorates, regardless of the path of IPF progression5
A line graph with disease progression on the y-axis with the labels onset of disease, onset of symptoms/pre-diagnosis period, diagnosis, and death. The x-axis shows time in years from 0 to 6 years.
Line A shows rapid disease progression. The line is straight, starting at onset of disease and ends at year 1.
Line B shows periods of relative stability punctuated by acute worsening or exacerbations. The line zigzags back and forth, starting at onset of disease and ends at year 3.
Line C shows gradual disease progression. The line is straight, starting at onset of disease and ends at year 6.
Line D shows stable disease progression. The line is straight, starting at onset of disease and ends at diagnosis. It does not reach death.
In IPF, baseline FVC doesn’t predict disease progression6,7

FVC has already declined before diagnosis7

Predicted FVC can appear to be greater than 100% at baseline7

Emphysema artificially increases FVC6,7

ILD is a common manifestation of SSc and a leading cause of death
For most patients with SSc-ILD, pulmonary involvement appears early, often developing into clinically significant lung disease within 3 years of diagnosis.19,20
It’s important to make an accurate diagnosis as early as possible,
regardless of the type of ILD.
CTD-ILD=connective tissue disease-associated interstitial lung disease; ILD=interstitial lung disease; SSc-ILD=systemic sclerosis-associated interstitial lung disease; iNSIP=idiopathic nonspecific interstitial pneumonia; HP=hypersensitivity pneumonitis; RA-ILD=rheumatoid arthritis-associated interstitial lung disease; pSS-ILD=primary Sjögren's syndrome-associated interstitial lung disease; cHP=chronic hypersensitivity pneumonitis;
PM-ILD=polymyositis interstitial lung disease; SLE-ILD=systemic lupus erythematodes interstitial lung disease; SS-ILD=Sjögren’s syndrome interstitial lung disease; MCTD-ILD=mixed connective tissue interstitial lung disease; FVC=forced vital capacity.
-
Wijsenbeek M, Cottin V. Spectrum of Fibrotic Lung Diseases: Supplementary Appendix. N Engl J Med 2020;383(10):958–68.
-
Flaherty KR, et al. Design of the PF-ILD trial: a double-blind, randomised, placebo-controlled phase III trial of nintedanib in patients with progressive fibrosing interstitial lung disease. BMJ Open Resp Res 2017;4(1):e000212.
-
Cottin V, et al. Presentation, diagnosis and clinical course of the spectrum of progressive-fibrosing interstitial lung diseases. Eur Respir Rev 2018;27:180076.
-
Pulmonary Fibrosis Foundation. What is pulmonary fibrosis? https://www.pulmonaryfibrosis.org/life-with-pf/about-pf. Accessed December 20, 2019.
-
Johannson KA, et al. Treatment of fibrotic interstitial lung disease: current approaches and future directions. The Lancet 2021;398(10309):1450–60.
-
Wijsenbeek M, Cottin V. Spectrum of Fibrotic Lung Diseases: Supplementary Appendix. N Engl J Med 2020;383(10):958–68.
-
Vancheri C, et al. Idiopathic pulmonary fibrosis: a disease with similarities and links to cancer biology. Eur Respir J 2010;35:496–504.
-
Park IN, et al. Clinical course and lung function change of idiopathic nonspecific interstitial pneumonia. Eur Respir J 2009;33:68–76.
-
Hyldgaard C, et al. A population-based cohort study of rheumatoid arthritis-associated interstitial lung disease: comorbidity and mortality. Ann Rheum Dis 2017;0:1–7.
-
Raimundo K, et al. Rheumatoid Arthritis–Interstitial Lung Disease in the United States: Prevalence, Incidence, and Healthcare Costs and Mortality. The Journal of Rheumatology 2019;46(4):360–71.
-
Bouros D, et al. Histopathologic Subsets of Fibrosing Alveolitis in Patients with Systemic Sclerosis and Their Relationship to Outcome. Am J Respir Crit Care Med 2002;165:1581–6.
-
Ito I, et al. Pulmonary Manifestations of Primary Sjögren’s Syndrome. Am J Respir Crit Care Med 2005;171:632–8.
-
Enomoto Y, et al. Prognostic Factors in Interstitial Lung Disease Associated with Primary Sjögren’s Syndrome: A Retrospective Analysis of 33 Pathologically–Proven Cases. PLoS ONE 2013;8(9):e73774.
-
Guler SA, et al. Heterogeneity in Unclassifiable Interstitial Lung Disease. Ann Am Thorac Soc 2018;15(7):854–63.
-
Hyldgaard C, et al. How does comorbidity influence survival in idiopathic pulmonary fibrosis? Respiratory Medicine 2014:108:647–53.
-
Vourlekis JS, et al. The Effect of Pulmonary Fibrosis on Survival in Patients with Hypersensitivity Pneumonitis. Am J Med 2004;116:662–8.
-
Nasser M, et al. Prevalence and mortality of systemic sclerosis-associated interstitial lung disease (SSc-ILD) using the Frenchnational health insurance system (SNDS) database in France. ERJ 2020;56:805.
-
Vancheri C. Common pathways in idiopathic pulmonary fibrosis and cancer. Eur Respir Rev 2013;22:265–72.
-
Tyndall AJ, et al. Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis 2010;69(10):1809–15.
-
Cottin V, Brown KK. Interstitial lung disease associated with systemic sclerosis (SSc-ILD). Respir Res 2019;20(1):13. doi: 10.1186/s12931-019-0980-7.
-
Morisset J, et al. The unmet educational needs of patients with interstitial lung disease. Setting the stage for tailored pulmonary rehabilitation. Ann Am Thorac Soc 2016;13(7):1026–33.